The first step in addressing seasonal allergies is asking “why is the immune system compromised?”
There can be various causes for a suboptimal immune system, and the reasons can vary from person to person. Ultimately, the goal is to identify and address the triggers and mediators in order to reduce inflammation and the production of histamine. Another thing to consider is your overall “histamine burden.” For those of us living in Arkansas, we are very aware of this potential “tipping point” every spring and fall. This burden may become excessive when certain pollens are being scattered into the air. These seasonal pollens will often “tip” a person into a histamine-fueled allergy attack. While addressing seasonal pollens is recommended, addressing the other causes of histamine release should also be done to reduce your histamine burden, and thus, reduce allergy symptoms.
What Is Histamine?
Histamine is an important part of your immune system that contributes to necessary inflammation during times of injury and healing. Histamine is released from your mast cells, which are present in every tissue in your body. Mast cells release multiple inflammatory mediators as part of your immune system response. Histamine is just one of these hundreds of mediators released by your mast cells.
Histamine is the inflammatory mediator that is mostly responsible for causing “allergic reactions.” It is incredibly powerful. For example, the smallest taste of a peanut in someone with a peanut allergy can trigger a strong histamine response. When histamine is unleashed, it sends inflammatory messages and signals throughout your body – to your throat, nose, gut, mouth, brain, skin, and lungs. And because of the widespread reach and impact of histamine, people can develop a multitude of symptoms.
Potential Histamine Triggers That Exacerbate Seasonal Allergies
Leaky Gut and an Imbalanced Gut Microbiome
An unhappy GI tract and imbalanced microbiome (dysbiosis) will contribute to GI inflammation, gut permeability (“leaky gut”) and an increase in HISTAMINE levels. Did you know that about 80% of your body’s immune cells reside along your GI tract? And that mast cells make up a significant part of these immune cells? Mast cells release histamine in response to food proteins that “leak” across the GI tract due to gut permeability. Also, the GI microbiome regulates histamine release and breakdown. Imbalanced gut bacteria can worsen this histamine response process. GI inflammation, dysbiosis, and gut permeability have many causes, mediators and triggers. Inflammatory diets comprised of processed foods are just one contributing factor. Stress, food intolerances, medications, poor sleep, and toxins all impact GI health and function, too.
Food Intolerances
This is a big one. Dairy intolerance is notorious for causing “allergies” — runny nose, stuffy nose, sinus congestion, sinus headaches, asthma, post nasal drip, etc. Wheat and/or gluten intolerance is another biggie. But, it’s important to note that any food can be problematic. Personally, I am unable to tolerate wheat, whey, eggs, honey, and cantaloupe. Anytime I eat these foods I experience an inflammatory response that includes a histamine reaction — diarrhea, itching, nasal congestion, increased heart rate, and sometimes anxiety, headaches, and nausea. The effects can last anywhere from an hour to over a day or more.
Did you know that children with behavioral issues such as ADD/ADHD are seven times more likely to have a food intolerance? Histamine is also a neurotransmitter. Excessive amounts of histamine can cause anxiety and concentration issues, in addition to sneezing, runny noses, nasal congestion, and itching. So, the symptoms of ADD/ADHD could be due to excessive histamine from an unhappy GI tract, leaky gut, and dysbiosis. Rule out food intolerances!!
NSAID and Ibuprofen Use
Just because anti-inflammatory medications are accessible over-the-counter, doesn’t mean these medications are benign and without any side effects. These medications can cause a leaky gut and GI inflammation, which in turn can cause increases in HISTAMINE levels. I see this time and time again in my practice. In fact, these medications just cause a vicious cycle of inflammation. Patients will take an NSAID (non-steroidal anti-inflammatory drug) for some type of pain. The NSAID will then contribute to GI inflammation, leaky gut, and an increase in histamine and other circulating immune complexes (CICs). Patients will then experience more pain from increased levels of histamine and other CICs and take another NSAID. The cycle then continues. Think twice before taking another dose of ibuprofen or NSAID.
Alcohol
Yep. Sorry to be the bearer of bad news. Especially with football season upon us. Alcohol can contribute to GI inflammation, which can increase histamine levels. Alcohol can have significant negative impacts on the GI microbiome. Even that glass of resveratrol-containing wine can contribute to dysbiosis. A glass here or there is probably inconsequential (depending on the size of your glass), but regular consumption of alcohol in all forms (beer, wine, martinis, scotch, etc.) will most assuredly cause some significant GI dysfunction and dysbiosis. However, it does appear that wine consumption causes less dysbiosis than beer and hard liquors, probably due to the antioxidant content of high quality wines.
Stress
Most people never consider stress as a trigger or mediator of their allergy symptoms. Stress, and the accompanying elevations in cortisol and adrenaline, always impact immune function. And not in a good way. Have you ever noticed that stressed out people tend to be sick more often? Not only will chronic stress lower your ability to fight off viral and bacterial infections, it can also increase the severity of allergy symptoms. Chronic stress often results in a decrease in digestive enzyme production and stomach acid levels. Inadequate enzyme and stomach acid production then leads to undigested food within the GI tract. Undigested food can cause lots of GI inflammation, dysbiosis, candida overgrowth, small intestinal bacterial overgrowth, etc. This scenario almost always causes an increase in histamine levels and, thus, an increase in histamine load.
Environmental Toxic Burden
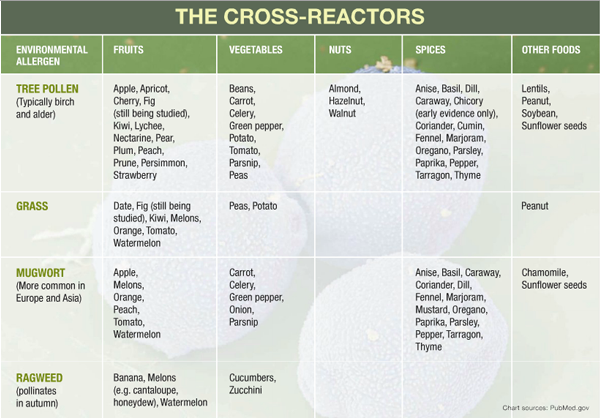
Molds, pet dander, dust, toxins, and pollen can contribute to your overall histamine burden. Beware of cross reactivity between certain pollens and foods. You can refer to the chart below. You’ll want to avoid certain foods during high pollen counts. For example, I avoid bananas during ragweed season, otherwise, I end up sneezing for the next couple of hours. Bananas cross-react with ragweed pollen. As do many other foods.
It’s also important to note that old government buildings and college dorms are notorious for having mold issues. I remember one patient who was “sick” Monday through Friday with symptoms of sneezing, headaches, sinus congestion, sore throat, and fatigue. But when the weekend rolled around her symptoms would improve. She said she could see the black mold on the ceiling and walls of her government building office.
Antibiotic Use
Sometimes antibiotics are necessary, but the misuse and overuse of antibiotics is contributing to some really imbalanced GI microbiomes. Antibiotics should be reserved for bacterial infections, but these “antibacterial medications” are being doled out for any inflammatory condition that arises. Antibiotics don’t just kill the offending bacteria causing the infection, they also kill many of the beneficial bacterial strains comprising your GI microbiome (and other biomes–lung, urogenital, skin, eyes, etc.). The risk of developing dysbiosis after antibiotic usage is very high.
In fact, antibiotic usage often precedes the onset of a variety of symptoms and “diagnoses” — IBS, eczema, sinusitis, asthma, depression, joint pain, autoimmune diseases, and many other conditions ending in “ism” and “itis.” This is especially true when broad-spectrum antibiotics are prescribed or when multiple rounds of antibiotics are used. The conditions and symptoms listed above are red flags for GI dysbiosis, and possibly, a leaky gut. When GI dysbiosis and/or a leaky gut is present, elevations in histamine levels are usually present, too. And you know what that means.
Lack of Dao Enzyme (Diamine Oxidase)
This enzyme is responsible for the breakdown of histamine. DAO is found in the thymus, kidneys, small intestine, and the placenta of pregnant women. Some people don’t make enough for different reasons — nutrient deficiencies and/or genetics play a role. Within the small intestine, DAO is responsible for the breakdown of food-derived histamine. Some foods have a high histamine content, some block the activity of DAO, and some liberate histamine. Supplementation with DAO is often recommended for people who are suspected of having this deficiency.
Cross-Reactors
Certain foods can “cross-react” with specific allergens and increase the severity of symptoms. When allergy season approaches, you may want to try eliminating the foods that could exacerbate the problem and increase your histamine burden.
How To Address Your Allergies with a Functional Medicine Approach
Here are some things I often recommend to my patients who suffer from allergies. Since the cause of allergies can be different from one person to the next, I recommend tailoring your approach to prioritize and address the causes you suspect or have identified.
1. Clean up your diet.
PRONTO. Avoid junk foods, processed foods, artificial sweeteners, and food dyes. Did you know artificial food dyes directly impact the activity of digestive enzymes? And not in a good way either. Eat unadulterated, minimally processed REAL FOOD. Go organic and avoid GMO foods. Take it easy on the alcoholic beverages, too.
2. Identify possible food intolerances by completing an Elimination and Reintroduction Diet.
This is the Gold Standard for identifying food intolerances, sensitivities, and allergies. Blood testing, skin testing, and colon biopsies often provide false positives and false negatives. An Elimination and Reintroduction Diet MUST be done correctly to get good data. Trust me, you will want to make sure you do it correctly because completion of this diet is not a walk in the park. Wheat, dairy, corn, soy, eggs, and nuts are the most common foods that give people problems, but you can have an intolerance/sensitivity to ANY food.
3. Avoid NSAIDs like ibuprofen and acid suppressing medications.
These can contribute to a leaky gut, GI inflammation, and elevations in HISTAMINE. But beware! There are MANY, MANY other medications that can negatively impact GI health and function.
4. Increase your intake of quercetin, a mast cell stabilizer.
Foods high in quercetin: citrus fruits, onions, apples, parsley, tea, tomatoes, broccoli, & lettuce. Quercetin is also available in an OTC capsule. You’ll want to make sure you don’t have an intolerance to the foods listed above. Citrus foods are known to be problematic for some people as they can “liberate” histamine. Quercetin is available in an OTC capsule. I know of several allergy and histamine intolerant patients that have been greatly helped by the regular use of quercetin supplementation.
5. Increase your intake of OMEGA 3 Fatty Acids.
These anti-inflammatory nutrients can also dampen down the histamine response. Foods high in OMEGA 3 FAs: cold-water fish (salmon, mackerel, anchovies, sardines), walnuts, flaxseed oil, grass-fed beef and eggs.
6. Try Stinging Nettle.
Stinging Nettle is a natural alternative to allergy medications. It works very similarly without the side effects. You will need to take it more often, though.
7. Use a Neti Pot.
Big advocate of this to clean the sinuses of pollens, dust, and other allergens. If my 6 yr-old nephew can do it, so can you. This has been shown to reduce the need for antihistamines for those with seasonal allergies. Be sure to use distilled water.
8. Take your shoes off before coming inside.
This will help you avoid bringing in pollens and dander. And it will help keep your house cleaner, too. And who doesn’t want a cleaner house?
9. Close the windows on windy days.
Dust and pollen can really getcha goin’. Also, clean and replace your filters regularly.
10. Look for mold in your home or work environment.
You’d be surprised by what you might find. Water leaks are notorious for causing a mold-loving environment. Old buildings are highly suspect. But even newly built homes can have problems. Remember, if you smell something “musty,” mold is likely present nearby.
**NOTE: You can find all of the aforementioned supplements at Fullscript, our online dispensary.

